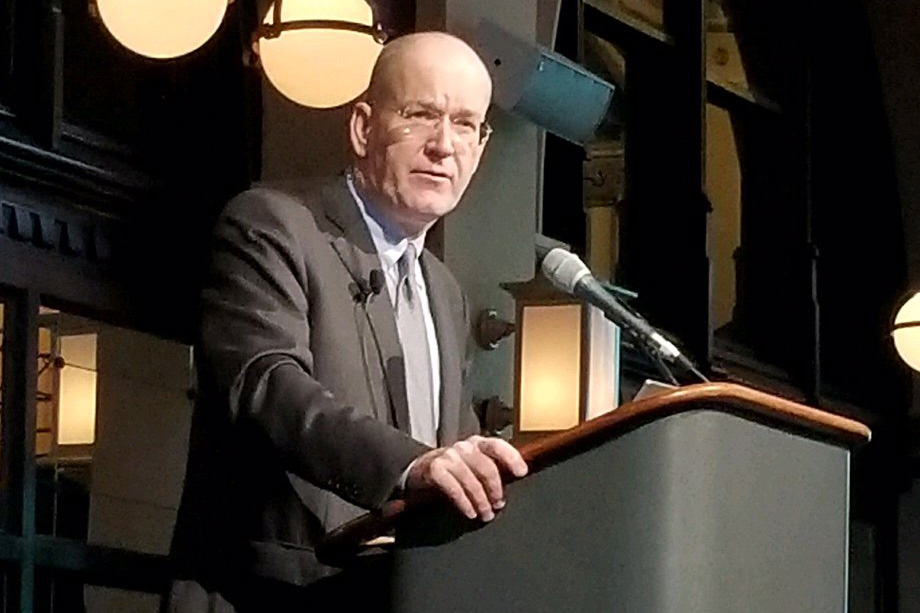
Rucker: Patient data access, choice is at heart of ONC rule
The Office of the National Coordinator for Health IT is pushing forward with a proposed rule meant to ensure patient access to their electronic healthcare information.
More for you
See AllLoading data for hdm_tax_topic #better-outcomes...